Numbers and evidence for a better health communication

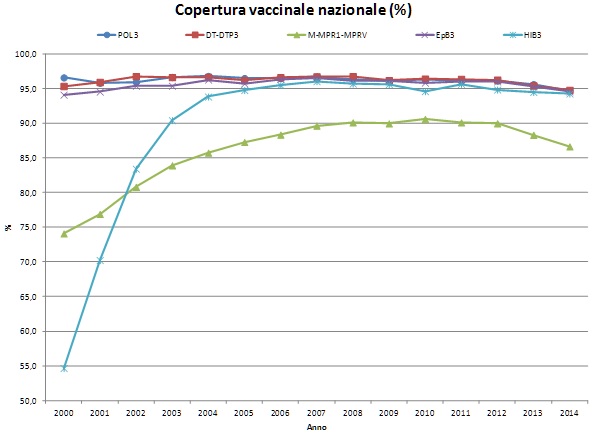
Italy is facing a serious drop in vaccine coverage, which are falling close to – and in some cases even below – the target set by the Minister of Health in the current national plan for vaccine prevention. This is a serious problem for public health, since, for infections transmitted from man to man (tetanus being an exception), a high coverage is necessary to protect those people that cannot be vaccinated either because of their age or because of clinical reasons, such as for cancer therapies, through the mechanism of herd immunity. Such a decline started in 2012 and involved all the vaccines, but it is wider for the measles-mumps-rubella vaccine, whose coverage has decreased by almost 4%, despite the presence of dedicated elimination plan in line with the official engagement subscribed by Italy at international level.
The decline can be inscribed within the phenomenon of vaccine hesitancy, which has been defined by the WHO experts as a kind of grey zone between full acceptance and outright refusal of all vaccines. WHO proposed three main determinants behind this hesitancy: the confidence in the source of the offer of vaccination and in the vaccine (effectiveness and safety); the convenience of the acceptance, defined as vaccination availability, affordability and accessibility; and the complacency towards the preventable infection due to the low risk perception of some vaccine-preventable diseases. These three factors may play different roles and have different weights depending on the context, but must be taken into account when planning public campaigns to support vaccination.
Doing that, however, requires a revised approach in terms of public health communication.
“Trying to face the decrease in vaccine coverages by simply relying on parents being scared by the diseases their children could get, is not effective anymore,” says Stefania Salmaso, head of the National Centre for Epidemiology, Surveillance and Health Promotion, within the Italian National Institute of Health, and member of the ASSET project. “Nowadays, many diseases disappeared and are not perceived as a real threat, thus, why vaccinating against a disease most of us had and survived (as measles, or rubella)? This is what complacency means. And this is why the fear of diseases cannot be the major argument to get vaccinated”.
Another common misconception, which in turn led to several communication mistakes, is the idea that vaccine hesitancy and refusal are driven only by a lack of knowledge of the target of the offer and therefore all the efforts are based on a one-way approach, trying to fill the gap. “It is not true,” claims Salmaso. “On the contrary, from some Italian surveys we know that vaccine refusal is more frequent amongst parents with higher educational qualification. It is thus clear that communication about vaccines cannot be a mere transfer of knowledge but has to address also other determinants of the choice”.
It is necessary to understand the context in which hesitancy or refusal arise and to get in touch with parents’ fears or believes. Ideally, we should tailor the communication on such issues to build a strong consensus on the right perception of the need of vaccination. For instance, hesitant individuals differ from the actual small percentage who refuse all vaccinations for ideological reasons, regardless of the scientific evidence. It is thus crucial to distinguish hesitancy from other reasons why people are unvaccinated or under-vaccinated, in order to mould communication efforts in the most proper direction. There is not a single communicative action that fits well in every situation.
“We have to recognize that our health system may not be properly organised to respond to individual needs, but it is also true that in Italy each child is registered with a caring doctor or a paediatrician hired by the national health service. These are powerful cultural mediators,” says Salmaso. “Being entrusted by families, they can fill the confidence gap between public and health institutions. However, their risk perception may be not that different from that of their patients as shown by the poor vaccination coverage among health staff”. This means that public health institutions should consider doctors as the primary target of the communication on vaccination. “The drop of vaccine coverage may indicate that there is also a gap between health authorities and healthcare workers themselves, who have not been trained to communicate with healthy people about prevention,” adds Salmaso.
For all these issues to be tackled, a change in the approach that drive health communication is thus required. A change that must rely on alliance building among health services and population based on transparency and on commonly defined health targets.
“To agree and set shared objectives is the only possible approach, when dealing with public health,” concludes Salmaso. “Communication must be carried out through numbers and evidence, giving all the available information and avoiding exaggerated claims, even if they are driven by good intentions. Pointing out the occurrence of cases or deaths should be made in respect to pre-defined and clearly stated health targets, agreed upon by the entire community. Only in these circumstances everybody (and not only health staff) should be engaged in meeting the target. Our success (or failure) in ordinary immunization program is a mark of what can be achieved during emergency situation like a pandemic, when we cannot expect to take advantage of confidence if we have not already gain it”.
